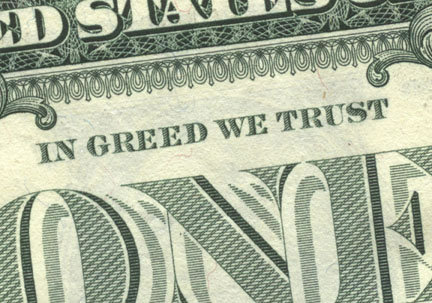
This may seem like a bit of a political rant that is only tangentially related to senior living but . . . here goes. A few days ago I read the last article in a three part series about hospice care published in the Washington Post titled Rising rates of hospice discharge in U.S. raise questions about quality of care and it made my blood boil.
Hospice as a Business
Providing hospice care can be a very lucrative business. Abusing the system (which means abusing the elders it serves) can make it even more lucrative. In order for an individual to receive hospice care, covered by Medicare, they must be diagnosed as having fewer than six months to live. The article makes some obvious points about hospice:
- When individuals enter hospice care their need for services is typically lower at the beginning than in the last few weeks and days before death.
- The further from death an individual begins hospice treatment the more profitable it is for the hospice agency.
- The healthier an individual on hospice, the lower the level of services needed, which means higher profits for the hospice agency.
- Figuring out when someone is six months from death is a very subjective process.
- On occasion, some hospice care recipients legitimately either take longer than six months to die or just plain defy medical odds and get better.
Hospice Abusing Elders . . . and the rest of us
One of the big challenges of a massive system like Medicare is that it is very difficult to control costs and fraud. So difficult, in fact, that most people who defraud the system make hundreds to millions of dollars and never get caught. When they do get caught the penalties are not sufficient to be much of a deterrent. I find myself thinking maybe the death penalty would be the right incentive . . . just kidding . . . sort of! According to the article there are two things happening
- There is a huge increase in the number of individuals who are being discharged from hospice. This likely means a couple of things: 1) That a significant number of individuals are being diagnosed as having less than six months to live when, in fact, that diagnosis was made only to open the hospice cash flow spigot. 2) As individuals are getting nearer to end of life, the quality of care deteriorates to the point that patients opt out of the hospice program at the time they need it most.
- In the last few weeks of life patients are being essentially forced off hospice care, often dumping them back into acute hospitals as a way to save the hospice companies the high costs of late stage care. This defeats every intended benefit of the Medicare hospice program: neither pain, suffering or money is saved.
These practices not only rip off the Federal government, your tax money and mine, they mean that residents are either being subjected to powerful drugs when they shouldn’t be or are not getting the services they most need in those last days.
Senior Living and Hospice Care
Hospice care has become an important part of senior living. It shifts some of the care cost for residents to the hospice and it allows residents to have longer lengths of stay. While good for the senior living community, it is also really good for residents, allowing them to spend their last weeks and days in a familiar, comfortable setting and, at the same time, to receive the pain medication needed to make their passing relatively painless. As an industry we have an obligation to vet the hospices that provide services to our residents. We need to refuse admittance to bad providers. Even more, we need to report those bad providers to the Office of the Inspector General. What has your hospice experience been like? Steve Moran
If you like this article (or even if you don’t) it would be a great honor to have you subscribe to our mailing list HERE





Steve,
I’ve been a healthcare administrator for over 25 years. I was fortunate that I participated in a hospital system that started a home health agency, hospice, home medical equipment company and a senior care facility. Since I was one of two licensed administrators, the development and operations was my responsibility. I must share, I loved the hospice experience~!
It was not an easy business to start in 1990. The clients and families did not want to give up hope of living, the Docs did not want to sign off on a death script (Their opinion at the time) and the staff was just getting to know what “Hospice and Palliative” care was. However, once all parties starting coming together….it was a beautiful care model to participate in.
Now, I’ve not been providing Hospice care for a number of years….but it is sad to hear of abuses taken place. I would hope that there are a few bad apples out in our industry, but as a whole….must providers are delivering hospice cafe as it was intended. Let’s not throw the baby out with the bath water….but do some pruning to get the problem providers out of the business.
Blessings,
Dr. B
Dr. B great reflections. Hospice is such a valuable thing for elders, families and senior living providers. It is shameful that some companies are abusing the system. I also worry that we will end up throwing the baby out with the bathwater.
Steve
Could you clarify something for me here? I’m not a provider. I’m a resident of a CCRC. Here’s my question: can a long term care facility offer its own hospice care (via the Medicare program) so that the patient (resident) doesn’t have to be physically moved to a different bricks and mortar hospice facility? If so, does Medicare then pick up the room rate, care costs, and meal costs? Being in a CCRC (Type C contract), I’ve seen family members move their loved one off site, one big motive being to NOT continue the billing costs of the SNF daily rate of the CCRC. If the SNF arm of the CCRC could say, “Keep your loved one here and receive the equal type of service and care than if you moved him/her to XYZ Hospice,” then the patient could stay on campus, among friends. I have cringed whenever I’ve seen a resident who moved through independent living to AL to the SNF, only to be moved off campus to a hospice facility across town when s/he reaches the end of the line. Couldn’t the SNF be reimbursed by Medicare when the resident gets the “hospice” classification? Wouldn’t that be best for the patient? Where does my thinking need to be corrected? Thanks.
Jennifer, what you’ve asked is complicated. Essentially, Medicare does not pay for residency in a nursing home. It will cover skilled care, i.e, rehab, but only for a short period of time. Medicaid, or the similar program in your state is the one that pays for the daily cost of care in a nursing home. Yes, a nursing home that provides hospice care would be reimbursed for all medical treatment of that resident. But the facility would still have to be paid for that room and board by Medicaid or the resident’s private resources. For that reason, many nursing homes will not provide hospice.
Thank you. I figured that was the case. There aren’t very many Medicaid cases in a CCRC; ours is not Medicaid certified. The family members are moving very sick patients into a hospice brick and mortar place where there is no charge for room and board, with the pocketbook in mind. Too bad the reimbursement system is such that a sick person has to be moved across town. Elderly friends in the CCRC then have a tougher time visiting, etc. I guess this means the brick and mortar hospice doesn’t have to charge for the room because it’s a “Hospice” versus a regular nursing home and they get Medicare money for the room and board? Or, is it a case of the community raising enough donations that the hospice facility doesn’t have to pass on the cost to the patient?
Milinda my sense is that many skilled nursing facilities allow hospices to come into the buildings to provide services.
Steve
Hi Jennifer:
I would start by suggesting you talk to the administration at your CCRC and asking them these questions. That being said, the Medicare Hospice program does not provide room and board. This means that a resident of either the skilled nursing component or the assisted living component might receive hospice care in those settings. The services would be paid for by Medicare (or perhaps by a Medicare Advantage HMO, I think). It would be additional services above and beyond the standard care being provided by the CCRC.
Steve
That is, if you have a responsible Administrator.
In my mother’s case, I was grateful that I was able to be with her at the last stages of her life. My mother was moved to hospital – Emergency, Christ Hospital, NJ from the Assisted Living Home (CCRC) where the Chaplain, Sister Nancy (a dream of a nun that I, thankfully, met seveal times while she was making her rounds in the hospital, made the right contacts for me to start paperwork for hospice.
I had no clue, not living in NJ and traveling back and forth from the West Coast, as to what steps to take for my mothers condition.
My mother was moved to Cusaks Care Center, in Jersey City, which had seveal rooms for Hospice that was administered by Compassionate Care. There were several shifts with several nurses, but I was most appreciative for the night nurse – Laverene Wessells -who, to this day, I am grateful to. She took the time to answer questions, guided me as to what steps were coming and on the last day of my mother’s life she discouraged me from going out to get a bite to eat. In her words “I would be surprised if your mother will still be here by the time my shift ends”. Sure enough, my mother’s breathing became more difficult, Laverne checked on her regularly, and stayed with me during the last moments of my mother’s life. She event told me what to expect at the end.
The doctor who came was busy prescribing more medication, didn’t say much, didn’t give me any information. It was Laverne who so compassionately guided me along the way.
None of this would have happened if my mother stayed at the Assisted Living Home where she was. The staff at the Infirmary would not have had the interest nor care that I experienced with Cusaks Care Center (they no longer have the hospice section due to Medicare changes), Compassionate Care and my ‘angel nurse’, Laverne.
Bianca great story of great care.
Steve
A person in a nursing facility does NOT have to move out to a hospice facility. They can and do receive the additional hospice services where they are living. A hospice aid can come in and help with ADL’s, just as if they were at home. They have the additional nursing services (hospice nurses are well trained in pain control). They can have the services of a social worker and a chaplain. The nursing home staff continue to care for them just as before. The hospice staff serves as an adjunt. They are available to give the families information and comfort as well.
Thanks Cheryl. A great concise description.
Steve
I used to be a huge proponent and supporter of hospice, in theory, in practice, and in policy. I still think that hospice has its place in the continuum of care, but it is not the beautiful concept once put in place by Elizabeth Khubler Ross.
Experience with multiple hospice agencies as an administrator of a 450 bed ALF was an exercise in frustration. Highlights of some of the problems: a hospice nurse decided without consult or checking the ALF chart for the resident that the resident no longer was safe at the ALF and moved to have him discharged and placed in a new facility where he would have been behind locked doors. The end of a long battle is that the resident stayed at our ALF, was carefully looked after and died in the only home he knew (due to dementia). The nurse was reported and the hospice instructed to never send her back to any of our residents. Another hospice nurse was overheard by a staff RN telling a resident (yes, I use and RN supervisor and every shift for each area of the ALF has licensed nurses for medication management, clinical assessment, and general quality control) who was very alert, and cognitively intact albeit dying from cancer, to “just sh1t in your diaper. I’m not going to help you get up by myself.” The hospice nurse never asked the ALF staff for assistance. The resident was crying and a passing staff member heard her and investigated. Another hospice worker (CNA) was observed by me, forcing a resident’s head back while clamping her mouth shut to get her to swallow. Now, there were incredibly wonderful and compassionate nurses, and cnas from hospice agencies, too however, we tend to get outraged by the abusive ones, and take the care from the good ones for granted. After all, it is their job to provide compassionate care.
In my personal life, hospice providing care to my terminally ill beloved relative was so poorly managed that she ended up breaking down, and died in excrutiating pain as the nurse could not manage the medications. A visit from a chaplain caused so much distress that another beloved family member ended up sobbing outdoors, as she’d been treated so badly by the so called chaplain.
A person in my family works for a hospice, one that was investigated for Medicare fraud. It was a terrible experience for all concerned. The CEO of that hospice told the staff that they were all getting what they deserved. He had made the decisions to fraudulently engage in billing practices, yet blamed it on staff.
So nope, I’m not a huge supporter any longer. I view hospice with a wary eye and am very cautious with my referrals to those agencies any longer. There is one (ONE) in my metropolitan area (where there are at least 9 hospices) that I will refer to at this time.
Poor service, lousy care and fraudulent billing practices. What happened to Elizabeth’s dream?
Eddie what a sad tale. Have had several people I was close to use hospice services in their last few weeks and it was in every case a very valuable useful service. I am fearful this will change and will take a great thing and destroy it.
Steve
I am sorry that you have had such terrible experiences with hospice employees. From the stories you tell, though, I am less ashamed of “hospice” as I am the nurses that came in and worked in your facility, with your residents. In the cases you describe, it is not the hospice that should have been alerted, but the boards of nursing in your state, overseeing the RN and CNA. We work hard for our licenses, and those who abuse or neglect patients need further education.
My professional and personal hospice experience has also been mixed. Professionally, I often had need to collaborate with local hospice agencies, all hospital run. There was only one that I could call that I knew would be out same day to do an eval. Sometimes, because MD’s won’t tell patients that they have exhausted their options, people die at home without what can be much needed and valued support – for their families. My personal experience when my mother was declining was gentle and supportive. The staff took cues from the family and my mom, we addressed issues that had been holding her up (family stuff), educated my siblings so I didn’t have to be “their nurse”, and took very good care of all of us.
Please take care in accusing any agency of fraudulent billing practices. Anyone who deals with government reimbursements can be called to account for billing errors, documentation omissions, etc. It would be as unfair as my saying that all ALF Directors are “snakes”, though I have certainly run into a few who put increasing care levels above resident needs and financial security….. I hope that you will heal through your past experiences, and that your local hospices will improve the communication/education of their nursing staff.
Katherine I need to start by saying that I have not been relating my experiences. In fact my hospice experiences have all be quite good. But the article points out a disturbing trend in statistics that suggests abuse. Great hospices should not feel at all offended or defensive about stories like this. Rather they should be part of the effort to expose and put out of business bad hospices.
Finally I agree that billing errors and document omissions do happen, but this trend is way beyond that.
Steve
As someone who has worked in the senior housing industry for nearly 3 decades, I have had numerous experiences with hospice services being provided to residents of communities over which I had charge. My take is that is imperative for the community (staff) to stay engaged with the residents’ care needs and wellbeing even when hospice becomes involved. Most if not all ALFs state that they will “coordinate” a resident’s healthcare (provides and services), this cannot stop simply because of a terminal diagnosis and the presence of a hospice provider. By staying involved with the resident, family, doctor and hospice provider, a community (staff) can head off problems, identify ones that exist and take action in the best interest of the resident, Senior living providers have an obligation that does not end when a resident is on hospice.
John some great comments and I would add to that, senior living providers must be willing to refuse bad hospice providers entrance to their communities.
Steve
In the ALFs that I manage, the resident who is receiving hospice services remains the resident of the ALF, and does not become the patient of the hospice. The problem from my perspective is that the hospice workers are not providing the services for which they are employed.
Our ALF teams remain fully engaged and involved in the resident’s care, quality of life, service delivery and satisfaction.
My husband and I own and operate a Board Certified Internal Medicine Practice, a 19 bed Directed Care Assisted Living Facility that takes medicaid (altcs) & an Assisted Living Locators Franchise. I am an RN & my husband is the MD. He has served as a Medical Director for Banner HH & Hospice and Hospice of the Valley here in the Phoenix area. We have seen the best of hospice care & staff and the worst, and everything in between. I have learned to communicate our expectations with the hospices we work with in our ALF. The medicare guidelines have changed completely in the last several years but these 2 hospices, and others, are still very helpful to our residents and their families. I know these are our caregivers favorites, and my spouse and I agree. They can be a huge benefit to our residents that qualify & their families. We are blessed here in AZ to have so many choices and the best of the best hospices. It is a extremely competitive market for them. Are they perfect? Absolutely not, but neither are we.
Rachelle, great words of wisdom. Good direction and oversight prevent many problems. I would just add, that if you have a hospice (or any outside vendor) that is doing a terrible job they should be dumped.
Steve
I’m now realizing that my wording was poor earlier. I know that hospice services are permitted inside the CCRC, ALF, or nursing home. But what I was referring to was the family deciding to move the patient OUT of the CCRC and into a hospice building because of cost. Evidently the community where I live has a strong hospice facility that has enough endowments that the room and board costs are either non-existent or significantly cheaper than the room rate at the SNF or ALF of the CCRC. My question has been answered: Medicare doesn’t pick up room and board, no matter where it is charged. A hospice facility (bricks and mortar) on the receiving end of lots of donations and memorials can provide the care via normal reimbursements of Medicare and the room and board costs are courtesy of the benevolent fund. It’s obviously worth it to family members to move someone across town.
Hi Jennifer. Thanks for the clarification.
Steve
When I was very young, I started working as a nurses aid. Back in those days, hospice was not an option for our residents; the nurses aids did everything for everyone. I got out of the business for years, and about 4 years ago, started back as a caregiver.
The first place I worked had 4 people on hospice. Bath aids, chaplains, social workers, and nurses came in and checked on the residents, and gave baths and changed meds and looked at wounds, etc., etc., etc. A couple of the caregivers I worked with hated the hospice aids, said they weren’t as gentle as they should be, and generally preferred to keep giving care themselves. I have been at a second ALF for about three years now, and let me tell you, the hospice people are amazing. The chaplain is gentle and kind, and loving, and has absolutely no problem weeping with families, or holding and hugging residents and families; the bath aids are gentle and loving, and I have watched several of them going above and beyond just giving baths; and the nurses who come out to our facility are well qualified, and there are really no words to describe them. Apparently, though, it wasn’t always this way. When our facility was built, and hospice first came out, there were a few terrible experiences. The owner and the administrator, along with the nurses, DEMANDED better people. One time in three years, we had a bath aid who probably shouldn’t have been a bath aid, much less working with hospice. She does not come out to our facility any more.
In the town where I live, there is a shiny new hospice facility. It is staffed mostly by volunteers, but also has paid staff. One of my neighbors has his wife there now, and they are blown away by the care she receives. She is in a comfortable (relatively speaking) bed, and there’s a bed for him to sleep in when she doesn’t want to sleep alone (they’ve been married for 22 years, so she doesn’t much like sleeping alone).
We have two hospitals in our town. The hospice facility is a part of the bigger of the two hospitals.
I live in a fairly small city. This is not Seattle or Phoenix size… but it also isn’t a one stop light town. We get a lot of migrant workers, and we have a lot of people whose first language isn’t English. I work in a small town 50 miles away.
Maybe the reason our hospice systems are so good is the fact that we aren’t in huge cities like Seattle or Phoenix or Portland or Los Angeles. In a smaller town, people watch what’s going on, and we notice when things are not right. That goes for the police, the health care, and in the health care, we especially notice what’s going on with our most vulnerable.
Sylvia you said it all in the one statement: “The owner and the administrator, along with the nurses, DEMANDED better people.”
I also agree that being in a smaller community makes it a lot more difficult to sustain a bad business.
Steve
hello steve……my experience working as a nurse in and with hospice has been generally very good. every health care organization learns the billing system and works within those parameters….there is most definitely fraud everywhere in healthcare, however, hospice care is an asset to families/people in need of end of life care….proud to have worked in the hospice arena. thank you and be well!
Marilyn. I think hospice is great. I just think we need to be aware that there seems to be a growth in shady practices by some hospice providers. Those providers need to be exposed and put out of business so that the hospice’s that are doing a great ethical job can continue to do what they do unimpeded by new regulations and stringent oversight.
Steve
Great article and conversation. I lived in an area in Florida where there was just one Hospice – so much for choice.
Hospice is my long term care plan. It is so wasteful to have VA, Medicaid, Medicare and Hospice all being funded to one extant or another by the U.S. Government.
An overhaul of consolidation through a continuum of care needs is in order.
The Hospice Palliative model is a good one- a multi therapeutic approach to pain and disease management with services for the whole family. Veteran’s can use it, Nursing Home residents can use it and any senior, so maybe it should folded into those departments or programs.
I still don’t fully understand how Hospice and Medicare Home Health are for profit when the government/taxpayers are footing the bill.
thanks for the discussion
They are for profit the same way that physicians are for profit, the way that consultants and contractors who do work for the government are for profit. I am always miffed by the slam of for profit entities. Without them there would be no one to pay taxes.
Steve
In the spring of 2013 both of my parents were placed on hospice care. My dad at the time was 92 and my mother 89. They both lived at home and, except for a few changes in medications and increased complaints of age-related discomforts, as far as I was concerned, they were doing OK. (Hmmm. Maybe I was in denial.) At the time, I didn’t understand why the doctor had them placed on hospice care, but after seeing the kind of care they received subsequently, I was comfortable with the decision. Oddly enough, they both passed away roughly within that magical six-month window – Dad while living at home and five weeks later, Mom, in an ALF to which we had admitted her since we would not have been able to safely care for herself and we did not have the bandwidth to be there with her 24X7. I was out of town at the AHCA convention last year just taking down our exhibit hall booth when I received the call about my father’s sudden, but I was able to be at my mother’s bedside when she passed away. Key to our family’s peace of mind was the understanding that patient and compassionate hospice workers were able to give us so that we could let Mom pass away with dignity and we could observe with peace and gratitude. I don’t know to this day how the doctor discerned the 6-month window, but to this day I am grateful and sing praises to the hospice agency and its workers.
Rand, a great testimony for hospice.
Steve